Tuberculous Abscess of the Anterior Abdominal Wall: An Unusual Site of Presentation
Awad Ali Mohamed Alawad and Mohamed Daffalla Gismalla
Cite this article as: BJMP 2016;9(4):a927
|
|
Abstract The skeletal muscles are rarely affected by tuberculosis (TB) because they are not a favourable site for the survival and multiplication of Mycobacterium tuberculosis. A case of tuberculous abscess in rectus abdominis muscle is described in a 20-year-old apparently healthy female with no past history of TB. The diagnosis was made by ultrasound-guided fine-needle aspiration and cytological examination which revealed caseating granuloma with central necrosis, lymphocytes, and giant cells, consistent with TB. After four weeks of antituberculous treatment, she responded well and the abscess regressed considerably. In most cases, the muscle involvement is secondary and caused by haematogenous route or direct inoculation from a tuberculous abdominal lymph node or extension from underlying tubercular synovitis and osteomyelitis. The objective of this study was to alert clinicians and radiologists of the possibility of TB when considering the differential diagnosis of any lesion even in any unlikely anatomical area, especially in those regions where TB is endemic. Keywords: Skeletal muscle tuberculosis, Intramuscular abscess, antituberculous drugs therapy |
Introduction
The skeletal type of muscles are rarely affected by tuberculosis (TB) because they are not a preferred site for the survival and multiplication of Mycobacterium tuberculosis.1 Even in patients with widespread involvement of the disease, TB rarely involves muscles. Petter et al recorded only one case of primary skeletal muscles TB in over 8,000 cases of all types of TB, with an incidence of 0.015%.2 Few cases of tubercular myositis have been described in literature until now, mostly in adults. This, together with the decline in TB in general, makes it unlikely that one would immediately consider TB as the cause of a rectus sheath abscess.
There are only limited cases reports of isolated tubercular involvement of the anterior abdominal wall even though TB is rampant in developing countries, and with the rapid spread of acquired immune deficiency syndrome (AIDS) it has made inroads into the developed nations as well.3 We are presenting a case of primary tuberculous abdominal wall abscess, with no evidence of pulmonary, skeletal or gastrointestinal TB in an immunocompetent patient. This case report should serve as a reminder that TB, in all of its various manifestations, remains very much among us.
Case report
A 20-year-old female presented to the outpatient department of surgery, with a complaint of a progressive swelling in the left lower abdomen for the last three months. There was no history of preceding trauma, fever, cough, malaise or pain. There was no history of contact with any case of TB. On examination, there was a swelling in the left iliac fossa, measuring 8x8cm in size, non-tender with smooth and ill-defined margins, and normal overlying skin. The swelling was firm in consistency and moved with respiration. Examination of the cardiovascular and respiratory systems were within normal limits.
Laboratory investigation revealed: haemoglobin 11.5 g/dl; total leukocyte count 8510/cumm with a differential count of 54% neutrophils, 42% lymphocytes and 4% eosinophils; erythrocyte sedimentation ratio 70 mm; and enzyme-linked immunosorbent assay (ELISA) for human immunodeficiency virus (HIV) negative. The chest radiograph was unremarkable. Other biochemical blood investigations, including liver and kidney function tests, were within normal limits. Ultrasonography of the abdomen revealed a 6.5x8.5cm left iliac fossa cystic mass with a liquefied necrotic centre in the anterior abdominal wall (Fig. 1). Computerized Tomography (CT) scan of the abdomen showed an abscess in the left antero-lateral portion of the abdominal wall limited to the muscle layer (Fig. 2). Ultrasound-guided fine-needle aspiration and cytological examination revealed caseating granuloma with central necrosis, lymphocytes, and giant cells, consistent with TB (Fig. 3). The patient was diagnosed to have tuberculous abscess of the anterior abdominal wall and antituberculous treatment was started following internal medicine consultation. She improved rapidly over the next few days. After four weeks of antituberculous treatment, she responded well to the treatment and the abscess regressed considerably. The patient did not require any surgical intervention.
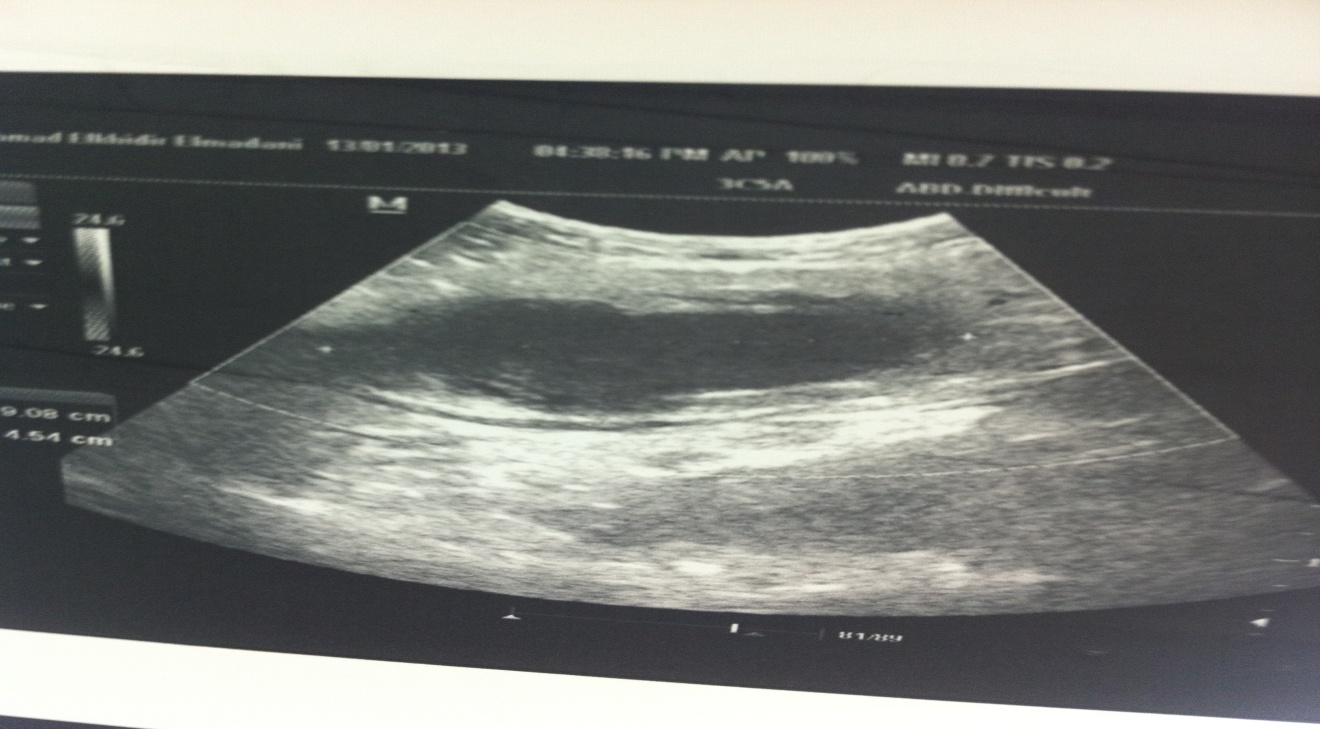
Figure 1. Ultrasonography of the abdomen revealed a left iliac fossa cystic mass.
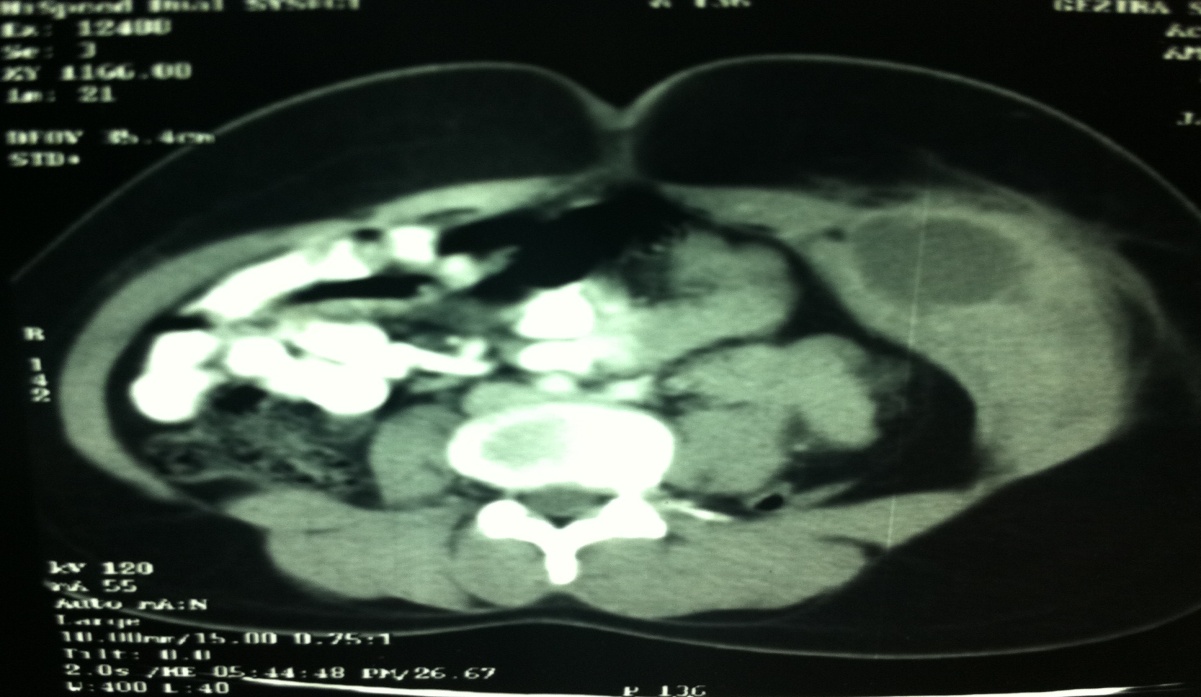
Figure 2. Focal cystic collection seen in the anterior abdominal wall of the left iliac fossa with mild peripheral enhancement (white arrow)
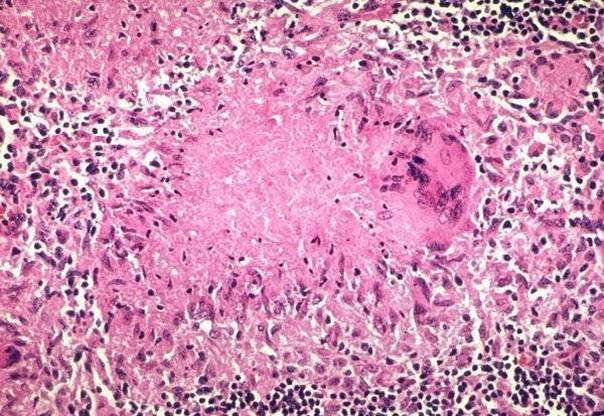
Figure 3. Photomicrograph revealed caseating granuloma with central necrosis, lymphocytes, and giant cells, consistent with tuberculosis.
Discussion
TB of the anterior abdominal wall is a rare entity and only isolated cases are reported in the literature. Possible explanation for the rarity of muscle involvement in TB includes high lactic acid content, lack of reticulo-endothelial tissue in muscle, lack of lymphatic tissue, the abundant blood supply, and the highly-differentiated state of muscle tissue.4 Although none of them seems to be an adequate explanation, all theories (except the first one) have been criticized.2
Two forms of skeletal muscle involvement are recognized.5 In the first type the tuberculous process spreads into the muscle through direct extension from a neighbouring structure e.g. bone, joint, tendon, or lymph node. In the second type the spread is haematogenous. Our patient is of interest because she seems to have a primary tubercular anterior abdominal muscular lesion with no evidence of immunoincompetence.
A tuberculous focus in the muscle usually manifests as progressive swelling and pain. The infection is usually restricted to one muscle.6 There may be a frank tuberculous abscess (as seen in our case) or a nodular sclerosis followed by calcification. Ultrasonography usually shows a cystic mass of mixed echogenicity with irregular walls and a liquefied, necrotic centre. Computed scan of the abdomen usually shows a well-defined abscess in the abdominal wall.7, 8 Ultrasonography or CT-guided aspiration followed by cytological examination usually reveals tuberculous granulomas with areas of caseous necrosis.
Management of this entity is mainly in the form of antituberculous drugs. Surgical intervention in the form of sonography, CT-guided aspiration or open drainage is usually reserved to patients where medical treatment has failed.3 Our patient responded well to medical treatment.
Although localized swelling in the rectus abdominis muscle is commonly due to necrotizing fasciitis, rectus sheath haematoma or tumours (benign / desmoid / malignant), a rare possibility of TB should also be considered. The prognosis is good in tuberculous myositis with appropriate chemotherapy.
Conclusion
This case alerts clinicians and radiologists of the possibility of TB when considering the differential diagnosis of any lesion even in any unlikely anatomical area, especially in those regions where TB is endemic.
|
Competing Interests None declared Author Details AWAD ALI MOHAMED ALAWAD, Assistant Professor, Department of Surgery, University of Medical sciences and Technology, Sudan. MOHAMED DAFFALLA GISMALLA, Assistant Professor, Department of Surgery, University of Gezira, Sudan. CORRESPONDENCE: Awad Ali Mohamed Ahmed Alawad, Department of Surgery, University of Medical Sciences and Technology, Sudan. Email: awadali82@hotmail.com |
References
- Sabat D, Kumar V. Primary tuberculous abscess of rectus femoris muscle: a case report. J Infect Dev Ctries. 2009;3(6):476-8.
- Malhotra MK. Cold abscess of the anterior abdominal wall: an unusual primary presentation. Niger J Surg. 2012 Jan;18(1):22-3.
- Rebai W, Chebbi F, Bouassida M, Azouz H, Ksantini R, Makni A, et al. [Tuberculosis of the abdominal wall: a rare localization]. Med Trop (Mars). 2010 Feb;70(1):6.
- Desai N, Patil S, Thakur BS, Das HS, Manjunath SM, Sawant P. Abdominal wall abscess secondary to subcapsular tubercular liver abscess. Indian J Gastroenterol. 2003 Sep-Oct;22(5):190-1.
- Saika A, Kanno T, Ishiguchi T, Oka H, Shiotani A, Yamanishi T, et al. [A case of the tuberculous abscess in the abdominal wall]. Kansenshogaku Zasshi. 1997 Jun;71(6):540-4.
- Abid M, Ben Amar M, Abdenadher M, Kacem AH, Mzali R, Mohamed IB. [Isolated abscess of the thoracic and abdominal wall: an exceptional form of tuberculosis]. Rev Mal Respir. 2010;27(1):72-5.
- Yilmaz T, Sever A, Gur S, Killi RM, Elmas N. CT findings of abdominal tuberculosis in 12 patients. Comput Med Imaging Graph. 2002 Sep-Oct;26(5):321-5.
- Sinan T, Sheikh M, Ramadan S, Sahwney S, Behbehani A. CT features in abdominal tuberculosis: 20 years experience. BMC Med Imaging. 2002 Nov 12;2(1):3.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




