Malignant Hypertension Masquerading as Thrombotic Thrombocytopenic Purpura
Muhammad Zohaib Bawany, Zeeshan Tariq, Thomas Sodeman and Anand Mutgi
Cite this article as: BJMP 2011;4(2):a418
|
|
Abstract Hypertension is common, but with early detection and treatment, it is rare to see malignant hypertension. Malignant hypertension is a medical emergency with an incidence of 1% in hypertensive patients. We report on a patient who presented with signs suggestive of Thrombotic Thrombocytopenic Purpura and severe hypertension, which resolved with the treatment of hypertension. Keywords: Malignant Hypertension, Thrombotic Thrombocytopenic Purpura |
INTRODUCTION:
Hypertension is common but, with early detection and treatment, it is rare to see malignant hypertension. We report a patient who presented with signs suggestive of thrombotic thrombocytopenic purpura and severe hypertension, which resolved with the treatment of hypertension.
CASE REPORT:
A 34 year old African American male presented to the emergency department (ED) having experienced nausea, vomiting and diarrhoea for two days. He denied haematochezia, meleana or sick contacts at home. He complained of blurred vision without photophobia, headache and mild chest discomfort. His past medical history was unremarkable. The patient did not have any significant family history. Smoking history was significant for a pack of cigarettes daily for seven years. He reported occasional alcohol intake, and denied use of recreational drugs. On presentation, this patient’s blood pressure was 201/151 mmHg, with a mean of 168 mmHg. Pulse 103 beats per minute, respirations 20 per minute and temperature 98.4F. Physical examination was otherwise unremarkable, including absence of focal neurological deficits.
Blood tests showed: Haemoglobin 12.6 g/dl, White cell count 13.9 g/dl, Platelets 67000, Sodium 136, Potassium 3.4, BUN 24, Creatinine 2.56 and LDH 556. Chest x-ray showed cardiomegaly. A non-contrast computed tomography scan of the brain did not show any sign of stroke (haemorrhage). Urinalysis was positive for proteins 4+, a large amount of blood, 0-2 white blood cells/high power field (HPF) and 0-2 red blood cells/HPF.
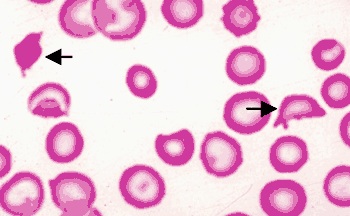
Figure 1
The patient’s initial treatment whilst in the ER consisted of a Labetalol drip. His mean arterial pressure decreased to approximately 115 mmHg during the first hour, and his chest pain and headache improved with the control of elevated mean arterial pressure. Furthermore, over the next 24 - 48 hours, the patient’s blood pressure was brought down to 138/86 mmHg and his blurred vision improved significantly. Subsequently, intravenous medications were switched to an oral regimen. Blood peripheral smear from the day of admission was significant for the schistocytes (Figure 1) suggesting ongoing haemolysis. Renal ultrasound was unremarkable. His cardiac ultrasound revealed an enlarged left ventricle, however no valvular abnormality was seen. Serum calcium and thyroid stimulating hormone levels were normal, as were urine catecholamines and vanillylmandelic acid level. On two week follow up in the outpatient clinic, the patient’s platelet count and creatinine had returned back to baseline and peripheral smear did not reveal any schistocytes as the blood pressure came under better control. [Table 1]
| Variable | On day 1 | Day 3 | Day 5 | Day 6 | Follow-up in 2 weeks |
| Haemoglobin | 12.6 | 9.3 | 9.3 | 10.3 | 11.4 |
| Platelets | 67, 000 | 65,000 | 90,000 | 125,000 | 204,000 |
| Retic. count | 3.9 | -- | -- | 4.3 | -- |
| Creatinine | 3.06 | 2.86 | 2.69 | 2.4 | 2.3 |
| BUN | 29 | 27 | 28 | 27 | 27 |
| LDH | 556 | 370 | 333 | 240 | -- |
| Troponin | 0.10 | 0.08 | 0.06 | 0.05 | -- |
| Peripheral Smear | Schistocytes | -- | -- | -- | No Schistocytes |
Table 1
DISCUSSION:
Malignant hypertension is a medical emergency with an incidence of 1% in hypertensive patients1and is more common in the African American population2. Depending on the clinical presentation, it must be differentiated from thrombotic thrombocytopenic purpura (TTP), disseminated intravascular coagulation (DIC), glomerulonephritis and vasculitis.
Suspicion for TTP was initially high in this patient because of haemolysis, thrombocytopaenia, central nervous system (CNS) manifestations and renal insufficiency. However, TTP did not explain the presence of elevated blood pressure3,4nor the improvement in symptoms and signs with the management of this, which clearly supports our diagnosis. Rapidly progressive glomerulonephritis did not explain the CNS symptoms, and a normal prothrombin time and activated partial thromboplastin time ruled against disseminated intravascular coagulation5. The patient did not have a history of preceding diarrhoea6, which could possibly direct towards haemolytic uraemic syndrome (HUS)4. There was no history of prosthetic valves, nor clinical evidence of vasculitis. The patient’s symptoms of severe hypertension, haemolysis, thrombocytopaenia and renal failure were consistent with malignant hypertension, and treating the hypertension7gradually resolved the thrombocytopaenia, haemolysis and renal failure8.
CONCLUSION:
This case report highlights that malignant hypertension is a medical emergency which can present with features resembling a wide variety of diseases, including TTP and HUS. Using appropriate management to control the elevation in blood pressure can help reveal the underlying diagnosis.
|
Competing Interests None declared Author Details Muhammad Zohaib Bawany MD, Zeeshan Tariq MD, Thomas Sodeman MD FACP, Anand Mutgi MD FACP, University of Toledo Medical Center, Toledo, OH CORRESPONDENCE: Muhammad Zohaib Bawany, University of Toledo Medical Center, 3000 Arlington Ave Mail stop 1150, Toledo OH, USA 43614 Email: Muhammad.Bawany@utoledo.edu |
References
1. Kitiyakara C, Guzman NJ. Malignant hypertension and hypertensive emergencies. J Am Soc Nephrol 1998;9:133-42.2. Khanna A, McCullough PA. Malignant hypertension presenting as hemolysis, thrombocytopenia, and renal failure. Rev Cardiovasc Med 2003;4:255-9.3. Patel A, Patel H. Thrombotic thrombocytopenic purpura: the masquerader. South Med J 2009;102:504-9.4. Shibagaki Y, Fujita T. Thrombotic microangiopathy in malignant hypertension and hemolytic uremic syndrome (HUS)/ thrombotic thrombocytopenic purpura (TTP): can we differentiate one from the other? Hypertens Res 2005;28:89-95.5. Kitchens CS. Thrombocytopenia and thrombosis in disseminated intravascular coagulation (DIC). Hematology Am Soc Hematol Educ Program 2009:240-6.6. Hertig A, Ridel C, Rondeau E. [Hemolytic uremic syndrome in adults]. Nephrol Ther 2010;6:258-71.7. Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest 2000;118:214-27.8. Gassanov N, Pollok M, Er F. Acute renal failure associated with malignant hypertension. Dtsch Med Wochenschr 2009;134:2224-7.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




