Bradyarrhythmias Associated with the Obstructive Sleep Apnoea Syndrome: A Precursor to Life-threatening Arrhythmias?
Amitasha Mann, Jean Karen Fleischman and Karen Mrejen-Shakin
Cite this article as: BJMP 2012;5(1):a511
|
|
Abstract Chronic Obstructive Pulmonary Disease (COPD) is a leading cause of global morbidity that is predicted to become the third most common cause of death worldwide by the year 20201. Obstructive sleep apnoea syndrome (OSAS) is also highly prevalent and is estimated to affect 5% of adults in western countries2. The co-existence of both COPD and OSAS in the same patient is termed the Overlap syndrome3,4. Overlap patients have more pronounced nocturnal hypoxemia and appear to be at increased risk of death compared with COPD patients matched for Global Initiative for COPD stage without OSA. We present a case of a patient with mild OSA and moderate COPD who was observed on CPAP titration polysomnography to have moderate obstructive sleep apnoea during rapid eye movement (REM) sleep (REM apnoea-hypopnea index (AHI) 28/hr.), with associated Wenckebach second-degree atrioventricular (AV) heart block observed during the nadir of oxygen desaturation associated with obstructive apnoeas. This led to further investigation with a one month event recording which showed progression of a benign Type I Wenckebach second-degree AV heart block to life-threatening Type II AV second-degree heart block and complete AV block with 3.9 seconds of ventricular asystole. Bradyarrhythmias during sleep observed in patients with COPD and OSAS may be a precursor to more life-threatening arrhythmias. |
Case Report
A 69 year old male with hypertension, body mass index 24 kg/m2, neck circumference 16 inches, and moderate COPD, on home oxygen, presented to his pulmonary clinic appointment with worsening complaints of fatigue, leg cramps, and intermittent shortness of breath with chest discomfort. A remote, questionable history of syncope five to ten years ago was elicited. His vital signs were: temperature 98.80F, blood pressure 119/76 mmHg, pulse 92/min and regular, and respirations 20/min. Physical exam was significant for crowded oropharynx with a Mallampati score of four, distant breath sounds with a prolonged expiratory phase on lung exam with a normal cardiac exam. Laboratory investigation showed normal complete blood counts, haemoglobin 15 g/dL, and normal chemistries. Compared to his previous studies, a pulmonary function study showed stable parameters with a FEV1 1.47 L (69%), FVC/FEV1 ratio 0.44 (62%), and a DLCO/alveolar volume ratio of 2.12 (49%). A room air arterial blood gas revealed pH 7.41, PCO2 44 mmHg, and PO2 61 mmHg, with 92% oxygen saturation. A six minute treadmill exercise test performed to assess the need for supplemental oxygen showed that he required supplemental oxygen at 1L/min via nasal cannula to eliminate hypoxemia during exercise. His chest radiograph was significant for hyperinflation and prominence of interstitial markings. A high resolution computed tomography of the chest demonstrated severe centrilobular and panacinar emphysema only. A baseline electrocardiogram (EKG) showed normal sinus rhythm with an old anterior wall infarct (Figure 1). Echocardiography of the heart revealed a normal left ventricle with an ejection fraction of 65%. Right ventricular systolic function was normal although elevated mean pulmonary arterial pressure of 55 mmHg was noted. A diagnostic polysomnogram performed for evaluation of daytime fatigue and snoring at night revealed mild OSA with an AHI of 6/hr. with sleep time spent with oxygen saturation below 90% (T-90%) of 19%. The EKG showed normal sinus rhythm. A full overnight polysomnogram for continuous positive airway pressure (CPAP) titration performed for treatment of sleep disordered breathing was sub-optimal, however it demonstrated an apnoea–hypopnea index (AHI) of 28 during REM (rapid eye movement) sleep, and a T-90% of 93%. The associated electrocardiogram showed Wenckebach second degree AV heart block during REM sleep usually near the nadir of oxygen desaturation. On a repeat positive airway pressure titration study, therapy with Bilevel pressures (BPAP) of 18/14 cmH20 corrected the AHI and nocturnal hypoxemia to within normal limits during Non REM (NREM) and REM sleep. His electrocardiogram remained in normal sinus rhythm .A twenty-four hour cardiac holter monitor revealed baseline sinus rhythm and confirmed the presence of second degree AV block of the Wenckebach type. A one month cardiac event recording showed normal sinus rhythm with frequent episodes of second degree AV block. These varied from Type I progressing to Type II with a 2:1 and 3:1 AV block, during sleep. Progression to complete heart block was noted with the longest pause lasting 3.9 seconds during sleep. The patient underwent an electrophysiology study with placement of a dual chamber pacemaker. He was initiated on BIPAP therapy. Subsequently, the patient was seen in clinic with improvements in his intermittent episodes of shortness of breath, fatigue, and daytime sleepiness.
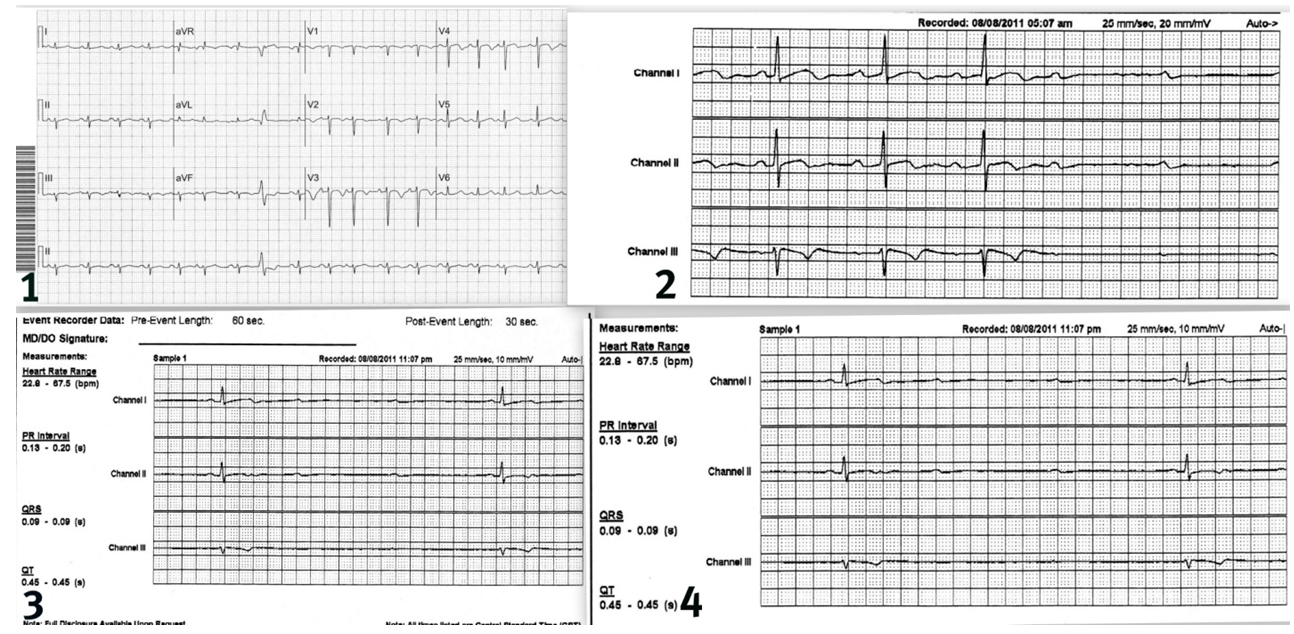
Figure 1- Patient’s baseline EKG, normal sinus rhythm. Figure 2 -Progression to Mobitz Type II block 5:07 am. Figure 3 and 4- Sinus pauses, longest interval 11:07 pm 3.9 seconds (Figure 4).
Discussion
In healthy individuals, especially athletes, bradycardia, Mobitz I AV block, and sinus pauses up to 2 seconds are common during sleep and require no intervention5. Cardiac rhythm is controlled primarily by autonomic tone. NREM sleep is accompanied by an increase in parasympathetic, and a decrease in sympathetic, tone. REM sleep is associated with decreased parasympathetic tone and variable sympathetic tone. Bradyarrhythmias in patients with OSA are related to the apnoeic episodes and over 80% are found during REM sleep. During these periods of low oxygen supply, increased vagal activity to the heart resulting in bradyarrhythmias may actually be cardioprotective by decreasing myocardial oxygen demand. This may be important in patients with underlying coronary heart disease.
Some studies have found that Mobitz I AV block may not be benign. Shaw6 et al studied 147 patients with isolated chronic Mobitz I AV block. They inserted pacemakers in 90 patients, 74 patients were symptomatic and 16 patients received a pacemaker for prophylaxis. Outcome data included five-year survival, deterioration of conduction to higher degree AV block, and new onset of various forms of symptomatic bradycardia. They concluded that survival was higher in the paced groups and that risk factors for poor outcomes in patients with Mobitz I included age greater than 45 years old, symptomatic bradycardia, organic heart disease, and the presence of a bundle branch block on EKG.
The Sleep Heart Health Study7 found a higher prevalence of first and second-degree heart block among subjects with sleep-disordered breathing (SDB) than in those without (1.8% vs. 0.3% and 2.2 vs. 0.9%, respectively). Gami et al8observed thatupon review of 112 Minnesota residents who hadundergone diagnostic polysomnography and subsequentlydied suddenly from a cardiac cause, sudden death occurred between the hours of midnight and 6:00 AM in 46% of those with OSA, as compared with 21% of those without OSA. In a study of twenty-three patients with moderate to severe OSA who were each implanted with an insertable loop recorder, about 50% were observed to have frequent episodes of bradycardia and long pauses (complete heart block or sinus arrest) during sleep9. These events showed significant night-to-night intra individual variability and their incidence was under-estimated, only 13%, by conventional short-term EKG Holter recordings.
Physiologic factors predisposing patients with OSA to arrhythmias include alterations in sympathetic and parasympathetic nervous system activity, acidosis, apnoea’s, and arousal2, 10, 11. Some patients with OSA may have an accentuation of the ‘Diving Reflex’. This protective reflex consists of hypoxemia-induced sympathetic augmentation to muscles and vascular beds associated with increased cardiac vagal activity which results in increased brain perfusion, bradycardia and decreased cardiac oxygen demand. In patients with cardiac ischemia, poor lung function (i.e. COPD), or both, it may be difficult to differentiate between these protective OSA-associated Bradyarrhythmias and those which may lead to sudden death. It has been well established that patients with COPD are at higher risk for cardiovascular morbidity12 and arrythmias13. Fletcher14 and colleagues reported that the effects of oxygen supplementation on AHI, hypercapnea and supraventricular arrhythmias in patients with COPD and OSA were variable. Out of twenty obese men with COPD studied, in most patients oxygen eliminated the bradycardia observed during obstructive apnoea’s and eliminated AV block in two patients. In some patients supplemental oxygen worsened end-apnoea respiratory acidosis however this did not increase ventricular arrhythmias.
CPAP therapy has been demonstrated to significantly reduce sleep–related Bradyarrhythmias, sinus pauses, and the increased risk for cardiac death 9, 15. Despite this, in certain situations placement of a pacemaker may be required. These include persistent life-threatening arrhythmias present in patients with severe OSAS on CPAP, arrhythmias in patients who are non-compliant with CPAP, and in patients who may have persistent sympathovagal imbalance and hemodynamic fluctuations resulting in daytime bradyarrhythmias16.
Our case is interesting since it highlights the importance of recognizing the association between OSA, COPD, and life-threatening cardiac arrhythmias. Primary care providers should note the possible association of OSA-associated bradyarrhythmias with life-threatening Type II bradyarrhythmias and pauses. Since bradyarrhythmias related to OSA are relieved by CPAP, one option would be to treat with CPAP and observe for the elimination of these arrhythmias using a 24hour holter or event recorder17. Compliance with CPAP is variable and if life-threatening bradycardia is present, placement of a permanent pacemaker may be preferred18.
Our patient is unusual because most studies showing a correlation with the severity of OSA and magnitude of bradycardia have included overweight patients without COPD19. This patient’s electrocardiogram revealed a Type II AV block at 5am (Figure 2). This is within the overnight time frame where patients with OSA have been observed to have an increased incidence of sudden death. Figures 3 and 4 show significant sinus pauses. In selected cases where patients have significant co-morbidities (i.e. severe COPD with OSA), in addition to treatment with positive airway pressure, electrophysiological investigation with placement of a permanent pacemaker may be warranted.
|
Competing Interests None declared Author Details Amitasha Mann MD Resident, PGY-2, Department of Medicine Jean Karen Fleischman MD, FCCP Associate Professor of Medicine Karen Mrejen-Shakin M.Sc, MD, FCCP Assistant Professor of Medicine Department of Medicine, Queens Hospital Centre N-Building, Room 707, 82-68 164th Street, Jamaica, NY 11432 CORRESPONDENCE: Amitasha Mann Department of Medicine, Queens Hospital Centre N-Building, Room 707, 82-68 164th Street, Jamaica, NY 11432 Email: amitashamann@gmail.com |
References
1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997; 349: 1498-1504.
2. Caples SM, Gami AS, Somers VK. Obstructive Sleep Apnea. Ann Inter Med 2005; 142: 187-197.
3. Lee R, McNicholas WT. Obstructive sleep apnea in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2011; 17: 79–83.
4. Marin JM, Soriano JB, Carrizo SJ, et al. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep: The overlap syndrome. Am J Respir Crit Care Med. 2010; 182: 325–331.
5. L.J.Gula, A.D. Krahn, A.C. Scanes, et al.Clinical Relevance of Arrythmias During Sleep: Guidance for Clinicians. Heart 2004 ; 90: 347-352
6. Shaw DB, Gowers JL, Kekwick CA, et al. Is Mobitz type I atrioventricular block benign in adults? Heart 2004 Feb; 90(2): 169-74.
7. Mehra R, Benjamin EJ, Shahar E, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med 2006; 173: 910-916.
8. Gami AS, Howard DE, Olson EJ, et al . Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 2005; 352: 1206-1214.
9. Simantirakis EN, Schiza SI, Marketou ME, et al. Severe bradyarrythmias in patients with sleep apnoea: the effect of continuous positive airway pressure treatment. A long-term evaluation using an insertable loop recorder. Eur Heart J. 2004 Jun; 25(12): 1070-6.
10. Narkiewicz K, van de Borne PJ, Pesek CA, et al. Selective potentiation of peripheral chemoreflex sensitivity in obstructive sleep apnea. Circulation 1999; 99: 1183–1189.
11. Narkiewicz K, van de Borne PJ, Cooley RL, et al. Sympathetic activity in obese subjects with and without obstructive sleep apnea. Circulation 1998; 98: 772–776.
12. S. Suissa, PhD et al. Cardiovascular Morbidity and Mortality in COPD. Chest 2005; 128: 2640-2646.
13. VG Tirlapur, et al. Nocturnal Hypoxemia and Associated electrocardiographic Changes in Patients with Chronic Obstructive Airways Disease. NEJM 1982; 306(3): 125-130.
14. NJ Alford, EC Fletcher, and D Nickeson. Acute Oxygen in patients with Sleep Apnea and COPD . Chest 1986; 89: 30-38.
15. Marin JJ, Carrizo SJ, Vicente E, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005; 365:1046–53.
16. Ki-Hwan Ji, MD, et al. Severe Obstructive Sleep Apnea with Symptomatic Daytime Bradyarrhythmia. Journal of Clinical Sleep Medicine. 2009; 5(3): 246-7.
17. Voigt L, Saul BI, Lombardo G, et al. Correction of AV- nodal block in a 27 year old man with severe obstructive sleep apnea – a case report. Angiology 2003 May-June; 54(3): 363-7.
18. Becker H, Brandenburg U, Peter JH, et al. Reversal of sinus arrest and atrioventricular conduction block in patients with Sleep Apnea during Nasal continuous positive pressure. Am J Resp Crit Care Med 1995; 151: 215-8.
19. Roche F, Thanh Xuong AN, Court-Fortune, et al. Relationship among severity of Sleep Apnea Syndrome, cardiac arrythmias, and autonomic imbalance. Pacing Clin Electrophysiology 2003; 26: 669-77.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




