Bednar tumour: an infrequent diagnosis
Manveen Kaur,Varsha Dalal and Anju Bansal
Cite this article as: BJMP 2015;8(4):a836
|
|
Abstract Bednar tumour is a pigmented variant of dermatofibrosarcoma protuberans (DFSP), constituting 1 to 5% of all DFSPs, which in turn, represent 0.1% of skin malignancies. It is histopathologically characterised by scattered melanosome-containing dendritic cells within an otherwise typical DFSP. Bednar tumour poses a clinical diagnostic challenge and requires histopathological and immunohistochemical examination to arrive at the correct diagnosis. We report a case of Bednar tumour occurring on the shoulder of a 29-year-old male. Keywords: Bednar, DFSP, pigmented tumour |
Introduction
Bednar tumour, first described by Bednar in 1957, is a pigmented variant of dermatofibrosarcoma protuberans (DFSP).It is a rare entity, constituting1 to 5% of all DFSPs, which in turn, represent 0.1% of skin malignancies. It differs from DFSP by the presence of dendritic cells containing melanin, interspersed between the fusiform cells characteristic of DFSP. The most frequent location is in the trunk followed by upper and lower extremities and the head and neck region. We report a case of Bednar tumour occurring on the shoulder of a 29-year-old male.
Case report
A 29 year old male patient presented with a slow-growing swelling on his left shoulder for the past two years. Physical examination revealed a large, nodular, subcutaneous mass measuring 8x7 cm in left suprascapular region. Clinical impression was of soft tissue tumour and total resection with 3-cm margins was performed. Grossly, tumour measured 9x4.5 cm, with grey white to grey black cut surface (Figure 1a, 1b). Microscopy showed spindled cells arranged in a tight storiform pattern admixed with scattered heavily pigmented cells (Figure 2). On immunohistochemistry, tumour cells were positive for vimentin and CD34 (Figure 3a, 3b) and negative for S100, SMA and desmin. Pigmented cells were found positive for S100 and HMB 45 (Figure 4a, 4b) and negative for other markers. Thus, a final diagnosis of Bednar tumour was rendered.
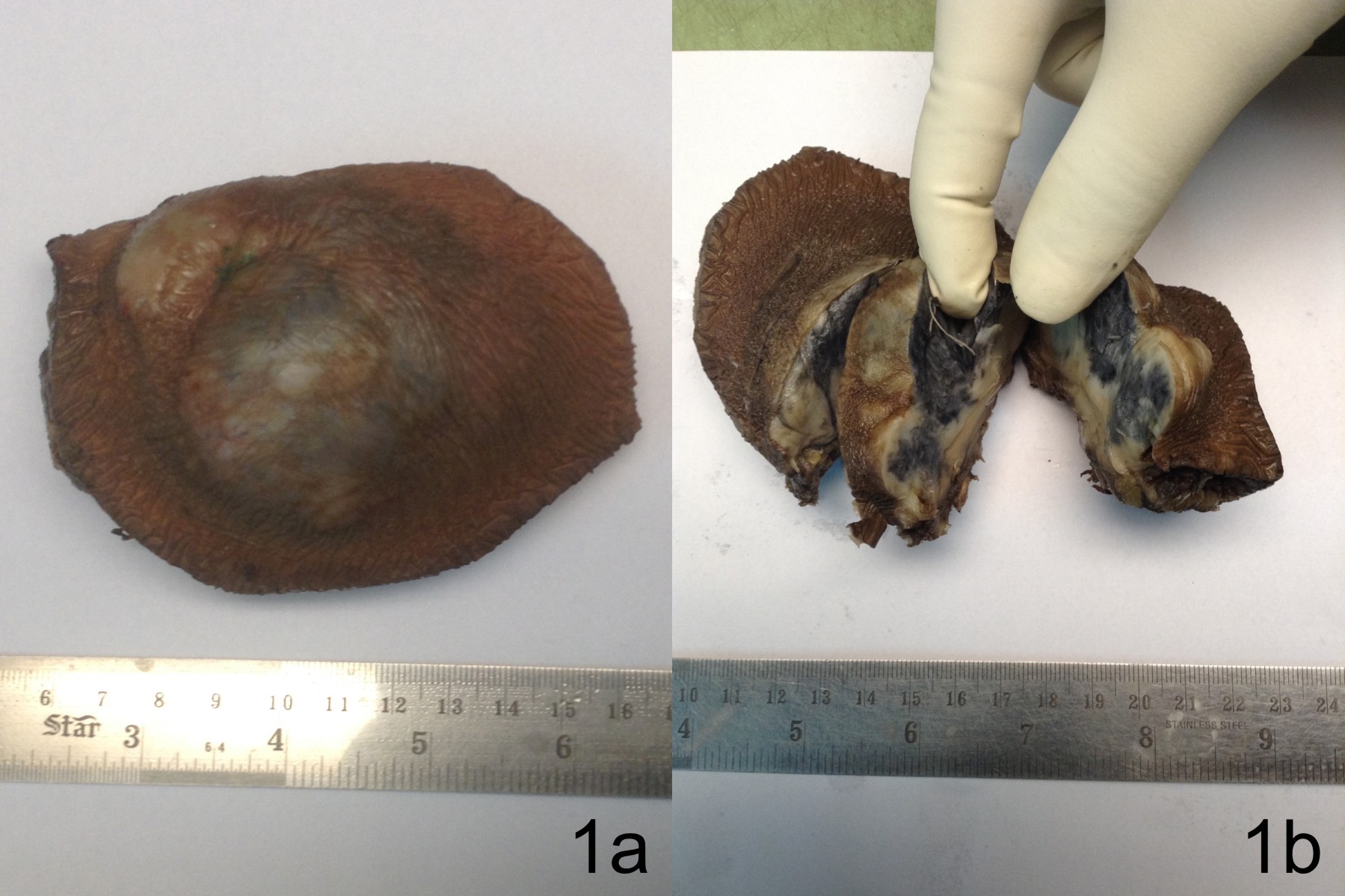
Figure 1 - Gross appearance of the tumour with cut surface grey white to grey black
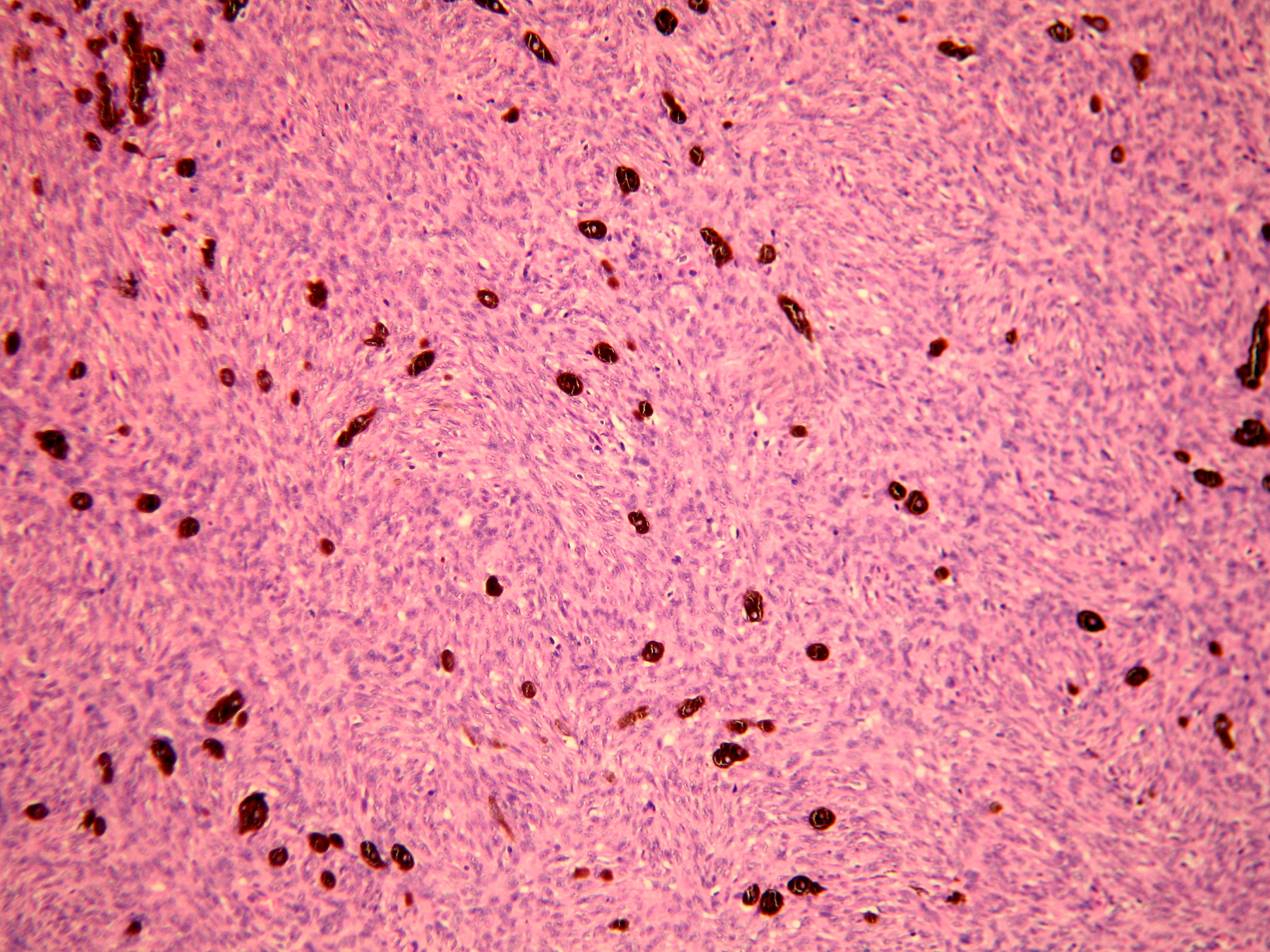
Figure 2 - Spindle cells in storiform pattern admixed with scattered heavily pigmented cells
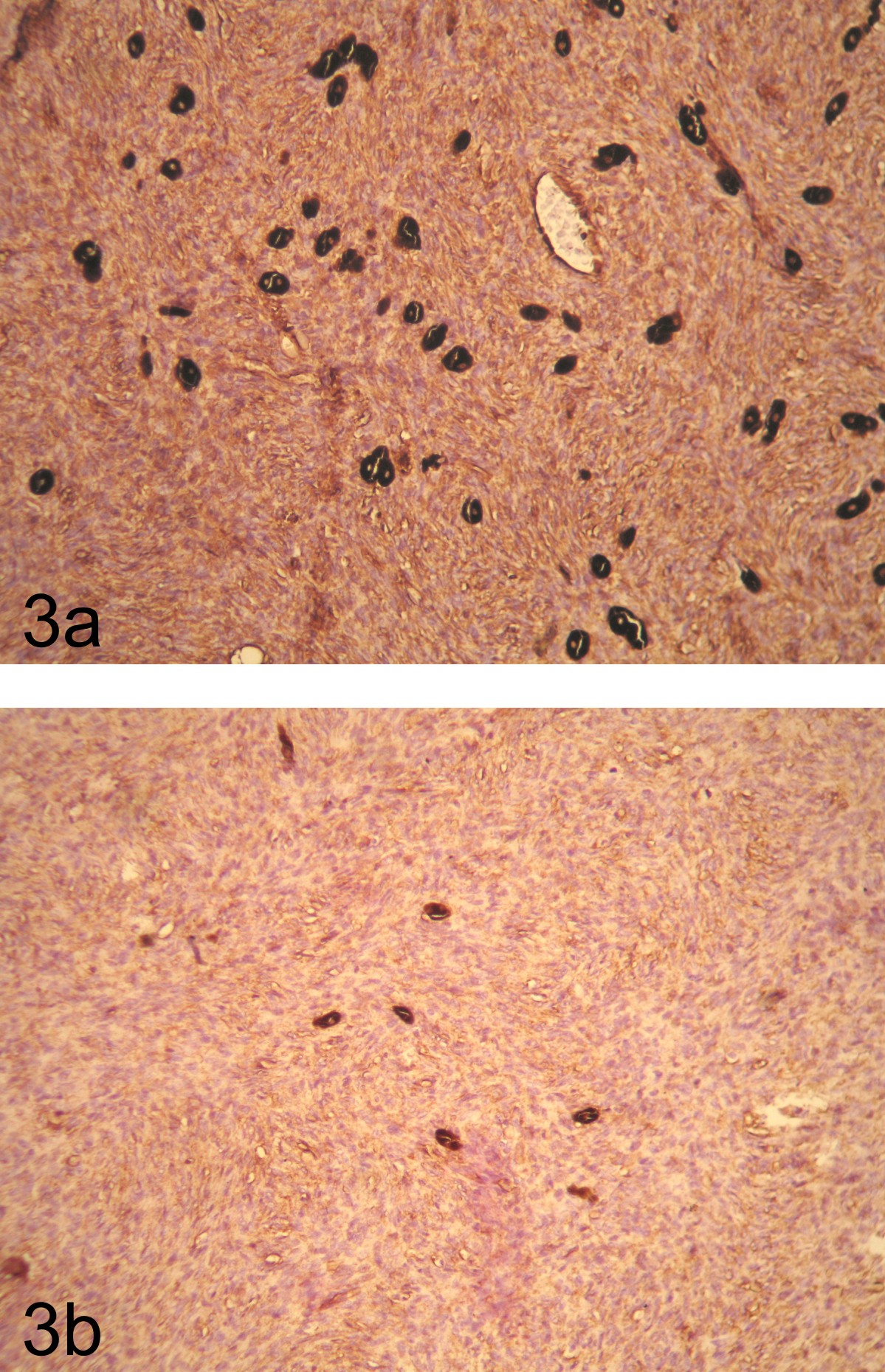
Figure 3 - Tumour cells were positive for vimentin (3a) and CD34 (3b)
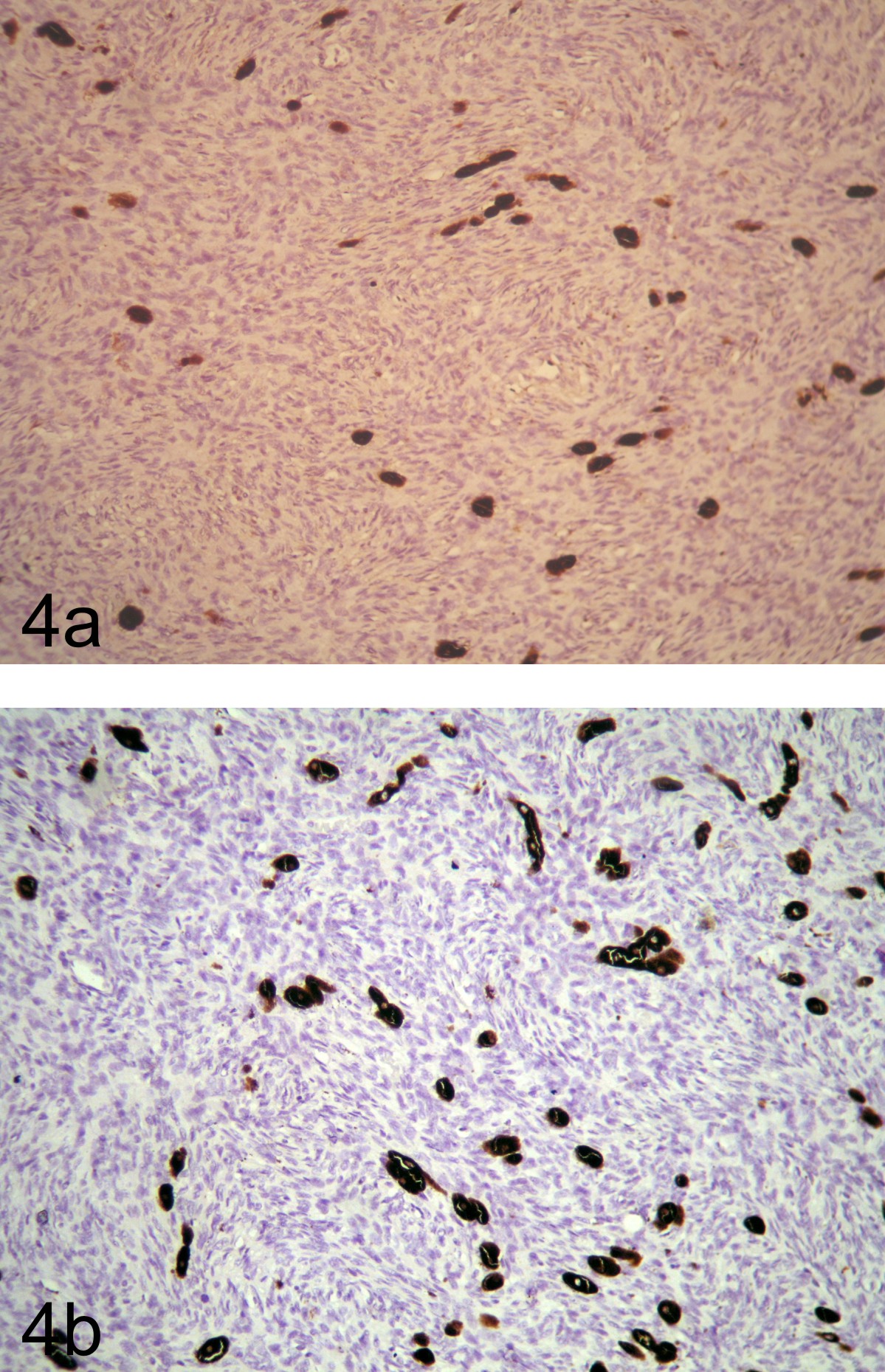
Figure 4 - Pigmented cells showed positivity for S100 (4a) and HMB 45 (4b)
Discussion
Dermatofibrosarcoma protuberans (DFSP) is a locally aggressive soft tissue neoplasm with intermediate malignant potential, regarded as a low grade sarcoma by the WHO classification of tumours of the skin.1,2,3
It was first described by Darier and Ferrand as a distinct cutaneous disease entity called progressive and recurring dermatofibroma in 1924. The term dermatofibrosarcoma protuberans was officially coined in 1925 by Hoffman.4
Histopathologically, DFSP is characterised by irregular, short, intersecting fascicles of tumour cells arranged in a characteristic storiform pattern. Cells have spindle-shaped nuclei which are embedded fairly uniformly in a collagenous stroma. There are several histological variants of DFSP. These include Bednar tumour, fibrosarcomatous, fibrosarcomatous with myoid/myofibroblastic change, myxoid, granular cell, palisaded, giant cell fibroblastoma, combined and indeterminate.5
Pigmented DFSP (Bednar tumour), first designated as storiform neurofibroma by Bednar, is a clinically and morphologicallydistinct variant of DFSP, constituting 5%-10% of all cases of DFSP.1,5 Clinical presentation is in the form of erythematous blue or brown coloured plaque lesions, with a smooth or irregular surface, often adhering to the deep tissue. The tumour may be exophytic, nodular or multilobulated and is generally firm in consistency.2 The lesions present as a slow growth, over a period of months or years. They have been described in all ethnic groups, with preponderance in blacks. They occur in third and fourth decades of life, however they may also occur in infancy and show a slight male predominance.1,5
The histogenesis of Bednar tumour is controversial. Some authors regard these tumours as being of neuroectodermal origin because of the presence of dendritic melanocytes and cells suggestive of Schwannian differentiation; while others believe attribute the origin to various kinds of local traumas, such as previous burns, vaccination scars, insect bites or vaccination such as BCG.3,6
Histopathologically, Bednar tumour is characterised by scattered melanosome-containing dendritic cells within an otherwise typical DFSP. The number of melanin-containing cells varies from case to case. Abundant pigmented dendritic cells can cause black discoloration of the tumor, whereas scant pigmented cells can be only identified microscopically.3,5 They grow invasively into the dermis and may reach the subcutaneous strata, fascia and musculature, in a manner similar to that of dermatofibrosarcoma protuberans. Occasionally, Bednar tumour may undergo fibrosarcomatous transformation with rare examples of pulmonary metastasis.5 Wang et al have reported a case of Bednar tumour with prominent meningothelial- like whorls.7
Immunohistochemically, most of the tumour cells stain positively with CD 34 and vimentin, and are negative for neuron-specific enolase, HMB-45 and protein S-100. However, cells containing melanin are positive for the usual melanocytic markers such as S-100 protein.5 On electron microscopy, three populations of cells have been identified, most of the cells being represented by fibroblasts. The second population exhibits fine elongations, enclosed in basal membrane while the third population consists of dendritic cells containing melanosomes and premelanosomes.3,5
The differential diagnoses include pigmented (melanotic) neurofibroma, psammomatous melanotic schwannoma, and desmoplastic (neurotrophic) melanoma. Pigmented neurofibroma can be differentiated from Bednar tumour by more extensive storiform growth and strong positivity for CD34 in latter. Psammamatous melanotic schwannoma is circumscribed, heavily pigmented with psammoma bodies, tumour cells being S- 100 positive and CD34 negative. Desmoplastic melanoma shows junctional activity and neurotropism.
Treatment consists of complete excision of the tumour with maximum preservation of normal tissue to maintain function and for optimal cosmesis. Moh’s Micrographic Surgery (MMS) or staged wide excision “Slow Moh’s “(with formal histopathological sectioning and delayed reconstruction for complete circumferential peripheral and deep margin assessment) has become the standard surgical treatment for DFSP.6,8
Bednar tumour presents a diagnostic challenge to the clinician because of resemblance to other commonly occurring pigmented lesions. Histopathological and immunohistochemical examination are necessary to arrive at the correct diagnosis.
|
Competing Interests None declared Author Details MANVEEN KAUR, MD (Pathology), Senior Resident,National Institute of Pathology (ICMR),Safdarjang Hospital Campus,New Delhi – 110029, India. VARSHA DALAL, MD (Pathology), Senior Resident, National Institute of Pathology (ICMR), Safdarjang Hospital Campus, New Delhi – 110029, India. ANJU BANSAL, MD (Pathology), Scientist D, National Institute of Pathology (ICMR), Safdarjang Hospital Campus, New Delhi – 110029, India. CORRESPONDENCE: DR ANJU BANSAL, MD (Pathology), Scientist D, National Institute of Pathology (ICMR), Safdarjang Hospital Campus, New Delhi – 110029, India. Email: dranjubansal@yahoo.com |
References
- Bednar B. Storiformneurofibromas of the skin, pigmented and nonpigmented. Cancer. 1957; 10:368-76.
- De Morais PM, Schettini APM, Chirano CA, et al. Bednartumor (pigmented dermatofibrosarcomaprotuberans): a case report. An Bras Dermatol. 2005;80(3):273-6.
- Weyers W, Mentzel T, Kasper RC, et al: Dermatofibrosarcomaprotuberans. In: World Health Organization Classification of Tumours. Pathology and Genetics of Skin Tumours. LeBoit PE, Burg G, Weedon D and Sarasain A (eds). IARC Press, Lyon, pp259-261, 2006.
- AboudKA. BlahoslavBednar (1916-1998) and the tumour which bears his name. Our Dermatol Online. 2012; 3(3): 239-240.
- Weiss SW, Goldblum JR. Bednartumor (pigmented dermatofibrosarcoma protuberance, storiformneurofibroma). Fibrohistiocytictumors of intermediate malignancy. Weiss &Goldblum eds. Enzinger and Weiss’s Soft Tissue Tumours, 5th ed. 2008, Mosby, Inc. P371-402.
- Llombart B, Serra-Guillén C, Monteagudo C, et al. Dermatofibrosarcomaprotuberans: a comprehensive review and update on diagnosis and management. Seminars in Diagnostic Pathology 2013; 30: 13-28.
- Wang J, Yang W. Pigmented dermatofibrosarcomaprotuberans with prominent meningothelial-like whorls. J CutanPathol 2008; 35 (Suppl. 1): 65–69.
- CampbellRM, ReganL, DufresneRG, et al. Bednar Tumor: Treatment With Mohs Micrographic Surgery. Cosmetic Dermatology 2006; 19(6): 422-4.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




